Type 1 diabetes, previously known as juvenile diabetes or insulin-dependent diabetes, is a chronic condition where the pancreas produces little to no insulin. Insulin is crucial as it allows sugar (glucose) to enter cells and produce energy. Factors such as genetics and certain viruses can contribute to the development of this condition. While it typically manifests during childhood or adolescence, it can also appear in adults. Despite extensive research, there is currently no cure for type 1 diabetes. Treatment focuses on managing blood sugar levels through insulin therapy, diet, and lifestyle changes to prevent complications.
Symptoms
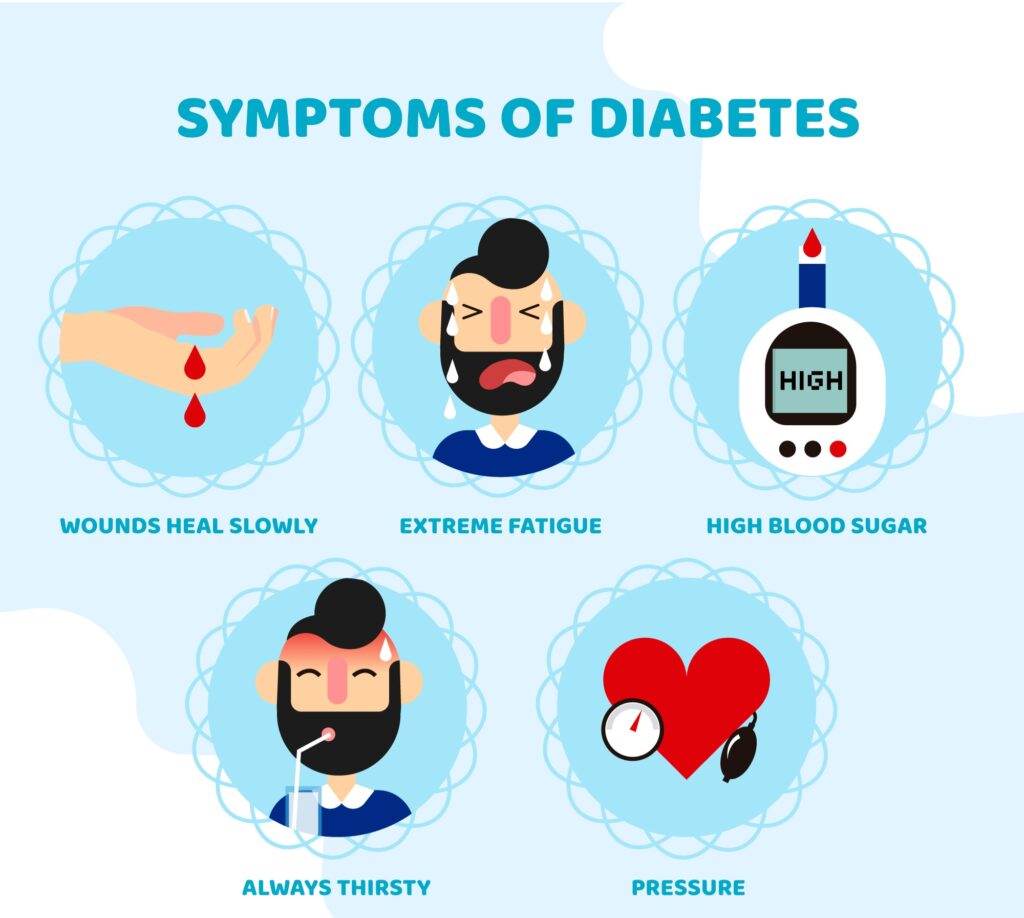
Symptoms of type 1 diabetes can develop suddenly and may include:
- Increased thirst
- Frequent urination
- Bed-wetting in children who previously did not wet the bed at night
- Extreme hunger
- Unintentional weight loss
- Irritability and other mood changes
- Fatigue and weakness
- Blurred vision
When to See a Doctor

Consult your healthcare provider if you or your child exhibit any of these symptoms.
Causes
The exact cause of type 1 diabetes is unknown. The immune system, which usually fights off harmful bacteria and viruses, mistakenly attacks and destroys the insulin-producing (islet) cells in the pancreas. Potential causes include:
- Genetics: Inherited traits may play a role.
- Environmental Factors: Exposure to viruses and other environmental elements may trigger the disease.
The Role of Insulin
Once a significant number of islet cells are destroyed, the body produces little or no insulin. Insulin is a hormone from the pancreas, a gland located behind and below the stomach.
- The pancreas releases insulin into the bloodstream.
- Insulin circulates through the body, allowing sugar to enter cells.
- Insulin reduces blood sugar levels.
- As blood sugar levels drop, the pancreas releases less insulin.
The Role of Glucose
Glucose, a type of sugar, is a primary energy source for the cells that make up muscles and other tissues.
- Glucose comes from food and the liver.
- Sugar is absorbed into the bloodstream and enters cells with the help of insulin.
- The liver stores glucose as glycogen.
- When glucose levels are low, the liver converts stored glycogen into glucose, maintaining typical glucose levels.
In type 1 diabetes, the absence of insulin prevents glucose from entering cells, leading to a buildup of sugar in the bloodstream and potential life-threatening complications.
Risk Factors
Several factors can increase the risk of developing type 1 diabetes:
- Family History: A parent or sibling with type 1 diabetes slightly raises the risk.
- Genetics: Certain genes are linked to a higher risk.
- Geography: The incidence of type 1 diabetes increases further from the equator.
- Age: Peaks in incidence occur in children aged 4-7 years and 10-14 years.
Complications
Long-term complications of type 1 diabetes can affect major organs, including the heart, blood vessels, nerves, eyes, and kidneys. Maintaining normal blood sugar levels can reduce the risk of complications, which can be disabling or life-threatening.
Heart and Blood Vessel Disease
Diabetes raises the risk of various cardiovascular issues, including coronary artery disease with chest pain (angina), heart attack, stroke, narrowing of the arteries (atherosclerosis), and high blood pressure.
Nerve Damage (Neuropathy)
Excess blood sugar can damage the walls of tiny blood vessels (capillaries) that nourish the nerves, especially in the legs. This can cause tingling, numbness, burning, or pain, starting at the tips of the toes or fingers and spreading upward. Poorly managed blood sugar can result in the loss of sensation in affected limbs. Nerve damage affecting the digestive system can lead to nausea, vomiting, diarrhea, or constipation, and in men, erectile dysfunction.
Kidney Damage (Nephropathy)
Diabetes can damage the kidneys’ filtering system, which consists of millions of tiny blood vessels. Severe damage can lead to kidney failure or irreversible end-stage kidney disease, requiring dialysis or a kidney transplant.
Eye Damage
Diabetes can harm the blood vessels in the retina (diabetic retinopathy), potentially causing blindness. It also increases the risk of other serious eye conditions, such as cataracts and glaucoma.
Foot Damage
Nerve damage or poor blood flow to the feet increases the risk of various foot complications. Left untreated, cuts and blisters can develop into serious infections, potentially leading to amputation of a toe, foot, or leg.
Skin and Mouth Conditions
Diabetes can make you more susceptible to skin and mouth infections, including bacterial and fungal infections. It also raises the likelihood of gum disease and dry mouth.
Pregnancy Complications
High blood sugar levels can pose risks for both the parent and the baby. Uncontrolled diabetes increases the risk of miscarriage, stillbirth, and birth defects. For the parent, it raises the risk of diabetic ketoacidosis, diabetic retinopathy, pregnancy-induced high blood pressure, and preeclampsia.
Prevention
Currently, there is no known way to prevent type 1 diabetes. However, researchers are working on ways to prevent the disease or protect islet cells in newly diagnosed individuals. Discuss with your healthcare provider the possibility of participating in clinical trials. It’s essential to carefully consider the risks and benefits of any experimental treatments.
summary
Engaging in a healthy lifestyle, including a balanced diet and regular physical activity, can help manage type 1 diabetes. Staying informed about new research and treatments, and maintaining regular check-ups with your healthcare team, are crucial steps in managing the condition effectively
By understanding type 1 diabetes better, individuals and families can take proactive steps to manage the condition and maintain a high quality of life
A Quick Review
Type 1 diabetes is a chronic condition where the pancreas produces little or no insulin, causing elevated blood sugar levels. It can develop at any age but commonly appears in childhood or adolescence. Symptoms include increased thirst, frequent urination, extreme hunger, and unexplained weight loss. Managing type 1 diabetes involves insulin therapy, diet, and lifestyle changes. While there’s no cure, effective management can prevent serious complications such as heart disease, nerve damage, and kidney issues.











